Other
Increased Delay from Atrial Fibrillation Diagnosis to Ablation Increases Mortality in Structural Heart Disease Patients
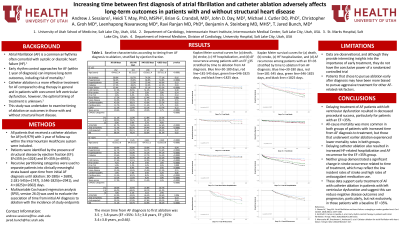
Purpose: Atrial Fibrillation (AF) is a common arrhythmia often comorbid with systolic or diastolic heart failure (HF). Catheter ablation is a more effective treatment for AF with concurrent left ventricular dysfunction, however, the optimal timing of use in these patients is unknown.
Material and Methods: All patients that received a catheter ablation for AF (n=9,979) with 1 year of follow-up within the Intermountain Healthcare system were included. Patients with were identified by the presence of structural disease by ejection fraction (EF): EF≤35% (n=1024), and 2: EF>35% (n=8955). Recursive partitioning categories were used to separate patients into clinically meaningful strata based upon time from initial AF diagnosis until ablation: 30-180 (n=2689), 2: 181-545 (n=1747), 3: 546-1825 (n=2941), and 4: >1825 (n=2602) days.
Results: The mean days from AF diagnosis to first ablation was 3.5 ± 3.8 years (EF >35%: 3.5±3.8 years, EF ≤35%: 3.4±3.8 years, p=0.66). In the EF >35% group, delays in treatment (181-545 vs. 30-180, 546-1825 vs. 30-180, >1825 vs. 30-180 days) increased the risk of death with a hazard ratio (HR) of 2.02 (p < 0.0001), 2.62 (p < 0.0001), and 4.39 (p < 0.0001) respectively with significant risks for HF hospitalization (HR:1.44-3.69), stroke (HR:2-01-2.14), and AF recurrence (HR:1.42-1.81). In patients with an EF ≤35%, treatment delays also significantly increased risk of death (HR:2.07-3.77) with similar trends in HF hospitalization (HR:1.63-1.09) and AF recurrence (HR:0.79-1.24).
Conclusions: Delays in catheter ablation for AF resulted in increased all-cause mortality in all patients with differential impact observed on HF hospitalization, stroke, and AF recurrence risks by baseline EF. These data favor earlier use of ablation for AF in patients with and without structural heart disease.
Material and Methods: All patients that received a catheter ablation for AF (n=9,979) with 1 year of follow-up within the Intermountain Healthcare system were included. Patients with were identified by the presence of structural disease by ejection fraction (EF): EF≤35% (n=1024), and 2: EF>35% (n=8955). Recursive partitioning categories were used to separate patients into clinically meaningful strata based upon time from initial AF diagnosis until ablation: 30-180 (n=2689), 2: 181-545 (n=1747), 3: 546-1825 (n=2941), and 4: >1825 (n=2602) days.
Results: The mean days from AF diagnosis to first ablation was 3.5 ± 3.8 years (EF >35%: 3.5±3.8 years, EF ≤35%: 3.4±3.8 years, p=0.66). In the EF >35% group, delays in treatment (181-545 vs. 30-180, 546-1825 vs. 30-180, >1825 vs. 30-180 days) increased the risk of death with a hazard ratio (HR) of 2.02 (p < 0.0001), 2.62 (p < 0.0001), and 4.39 (p < 0.0001) respectively with significant risks for HF hospitalization (HR:1.44-3.69), stroke (HR:2-01-2.14), and AF recurrence (HR:1.42-1.81). In patients with an EF ≤35%, treatment delays also significantly increased risk of death (HR:2.07-3.77) with similar trends in HF hospitalization (HR:1.63-1.09) and AF recurrence (HR:0.79-1.24).
Conclusions: Delays in catheter ablation for AF resulted in increased all-cause mortality in all patients with differential impact observed on HF hospitalization, stroke, and AF recurrence risks by baseline EF. These data favor earlier use of ablation for AF in patients with and without structural heart disease.