Cardiac: Other
Association Between Active Esophageal Cooling And Increased Procedural Volumes Of Catheter Ablation
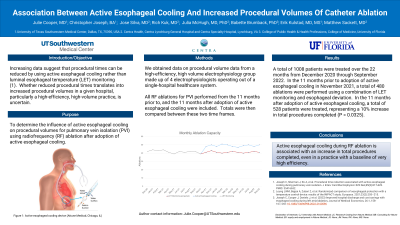
Purpose: To determine the influence of active esophageal cooling on procedural volumes for pulmonary vein isolation (PVI) using radiofrequency (RF) ablation after adoption of active esophageal cooling. Increasing data suggest that procedural times can be reduced by using active esophageal cooling rather than luminal esophageal temperature (LET) monitoring. Whether reduced procedural times translates into increased procedural volumes in a given hospital, particularly a high-efficiency, high-volume practice, is uncertain.
Material and Methods: We obtained data on procedural volume data from a high-efficiency, high volume electrophysiology group made up of 4 electrophysiologists operating out of a single-hospital healthcare system. All RF ablations for PVI performed from the 11 months prior to, and the 11 months after adoption of active esophageal cooling were included. Totals were then compared between these two time frames.
Results: A total of 1008 patients were treated over the 22 months from December 2020 through September 2022. In the 11 months prior to adoption of active esophageal cooling in November 2021, a total of 480 ablations were performed using a combination of LET monitoring and esophageal deviation. In the 11 months after adoption of active esophageal cooling, a total of 528 patients were treated, representing a 10% increase in total procedures completed (P = 0.0325).
Conclusions: Active esophageal cooling during RF ablation is associated with an increase in total procedures completed, even in a practice with a baseline of very high efficiency.
Material and Methods: We obtained data on procedural volume data from a high-efficiency, high volume electrophysiology group made up of 4 electrophysiologists operating out of a single-hospital healthcare system. All RF ablations for PVI performed from the 11 months prior to, and the 11 months after adoption of active esophageal cooling were included. Totals were then compared between these two time frames.
Results: A total of 1008 patients were treated over the 22 months from December 2020 through September 2022. In the 11 months prior to adoption of active esophageal cooling in November 2021, a total of 480 ablations were performed using a combination of LET monitoring and esophageal deviation. In the 11 months after adoption of active esophageal cooling, a total of 528 patients were treated, representing a 10% increase in total procedures completed (P = 0.0325).
Conclusions: Active esophageal cooling during RF ablation is associated with an increase in total procedures completed, even in a practice with a baseline of very high efficiency.