Cardiac: Other
Modified Atrial Fibrillation Burden: A Novel Metric to Account for Both Rhythm and Rate Control
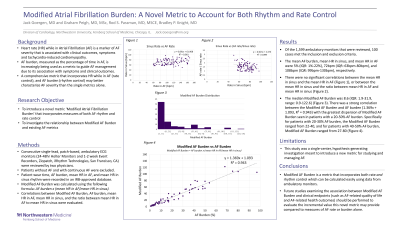
Purpose: Atrial fibrillation (AF) burden is increasingly being used as an endpoint in AF management. A comprehensive metric that accounts for the degree of both rate and rhythm control may be a better metric than AF burden. The objective of the present study is to derive a new metric termed ‘Modified AF Burden,’ which encapsulates both rhythm and rate control to further assess AF severity.
Material and Methods: Consecutive single-lead, patch-based, ambulatory ECG monitors (24-48 hour Holter Monitors and 1-2 week Event Recorders, Ziopatch, iRhythm Technologies, San Francisco, CA) were reviewed by two physicians. Patients without AF and those with continuous AF were excluded. Patient wear time, AF frequency, average HR in AF, and average HR in sinus rhythm were recorded in an IRB-approved database. Associations between AF burden, average HR in AF, and average HR in sinus were evaluated. Modified AF Burden was calculated using the following formula: AF burden x (average HR in AF/average HR in sinus).
Results: Of the 1,599 ambulatory monitors that were reviewed, 100 cases met the inclusion and exclusion criteria. The median AF burden, median average HR in sinus, and median average HR in AF were 5% (IQR: 1%-22%), 72bpm (IQR: 63bpm-80bpm), and 108bpm (IQR: 99bpm-130bpm), respectively. There were no significant correlations between the average HR in sinus and the average HR in AF (y = 0.091x + 61.908, R² = 0.0609), or between the average HR in sinus and the ratio between average HRs in AF and sinus (y= -0.0127x + 2.4728, R² = 0.0998). Furthermore, there was no significant correlation between AF burden and the ratio between the average HRs in AF and sinus (y = -0.0045x + 1.6279, R² = 0.0459). The median Modified AF Burden was 8.6 (IQR: 1.9-31.9, range: 0.85-122.6). There was a strong correlation between the Modified AF Burden and AF burden (1.3686x + 1.0928, R² = 0.943) with the greatest dispersion of Modified AF Burden seen in patients with a 20-50% AF burden. Specifically for patients with 20-30% AF burden, the Modified AF Burden ranged from 22-40, and for patients with 40-50% AF burden, Modified AF Burden ranged from 27-80.
Conclusions: Modified AF Burden can be calculated easily using data from ambulatory monitor reports. Future studies are needed to determine whether Modified AF Burden correlates better with AF-related quality of life and relevant clinical endpoints compared to AF burden alone.
Material and Methods: Consecutive single-lead, patch-based, ambulatory ECG monitors (24-48 hour Holter Monitors and 1-2 week Event Recorders, Ziopatch, iRhythm Technologies, San Francisco, CA) were reviewed by two physicians. Patients without AF and those with continuous AF were excluded. Patient wear time, AF frequency, average HR in AF, and average HR in sinus rhythm were recorded in an IRB-approved database. Associations between AF burden, average HR in AF, and average HR in sinus were evaluated. Modified AF Burden was calculated using the following formula: AF burden x (average HR in AF/average HR in sinus).
Results: Of the 1,599 ambulatory monitors that were reviewed, 100 cases met the inclusion and exclusion criteria. The median AF burden, median average HR in sinus, and median average HR in AF were 5% (IQR: 1%-22%), 72bpm (IQR: 63bpm-80bpm), and 108bpm (IQR: 99bpm-130bpm), respectively. There were no significant correlations between the average HR in sinus and the average HR in AF (y = 0.091x + 61.908, R² = 0.0609), or between the average HR in sinus and the ratio between average HRs in AF and sinus (y= -0.0127x + 2.4728, R² = 0.0998). Furthermore, there was no significant correlation between AF burden and the ratio between the average HRs in AF and sinus (y = -0.0045x + 1.6279, R² = 0.0459). The median Modified AF Burden was 8.6 (IQR: 1.9-31.9, range: 0.85-122.6). There was a strong correlation between the Modified AF Burden and AF burden (1.3686x + 1.0928, R² = 0.943) with the greatest dispersion of Modified AF Burden seen in patients with a 20-50% AF burden. Specifically for patients with 20-30% AF burden, the Modified AF Burden ranged from 22-40, and for patients with 40-50% AF burden, Modified AF Burden ranged from 27-80.
Conclusions: Modified AF Burden can be calculated easily using data from ambulatory monitor reports. Future studies are needed to determine whether Modified AF Burden correlates better with AF-related quality of life and relevant clinical endpoints compared to AF burden alone.